Causes, Prevention and Treatment of Fat Necrosis after Mastopexy
Fat necrosis is a condition characterised by the death of fatty tissue in the breast. It occurs when the blood supply to a portion of the fat cells is disrupted, causing the cells to die. This can result in the formation of firm lumps or nodules within the breast tissue. The condition is not harmful, but fat necrosis can cause physical changes that may be concerning.
At Dr Jake Lim’s practice, patient education is a priority. Dr Lim is dedicated to helping patients make decisions about their breast lift – mastopexy procedure by providing detailed information about potential risks of the procedure, including fat necrosis.
Download Dr Lim’s Breast Lift – Mastopexy Surgery Guide

How Does Fat Necrosis Manifest?
Fat necrosis often presents as a lump or nodule in the breast, which may feel firm or rubbery. The size and shape of the lump can vary, and it may or may not be painful. In addition to lumps, other symptoms may include:
- Skin Changes: The skin over the affected area may appear dimpled, bruised or red. These changes can sometimes resemble those seen in other breast conditions, making it important to differentiate.
- Firmness: The lump or nodule is often firm and may be mobile when touched.
- Pain or Tenderness: Some women experience discomfort or tenderness, while others may not feel any pain at all.
- Nipple Discharge: Though less common, fat necrosis can cause nipple discharge if it affects tissue near the nipple.
Causes of Fat Necrosis after a Breast Lift – Mastopexy
The causes can generally be categorised into surgical factors, patient-related factors, and the use of fat grafting during the procedure.
Surgical Factors
The most significant cause of fat necrosis in breast lift surgery is related to the disruption of blood supply during the operation. Here’s how it happens:
- Blood Supply Disruption: During a breast lift – mastopexy, Dr Lim removes excess skin and repositions the breast tissue to achieve a more lifted appearance. This process involves making incisions and separating tissues, which can disrupt the blood vessels that supply the fatty tissue within the breast. If the blood flow to these fat cells is compromised, it can lead to cell death, resulting in fat necrosis. The greater the extent of the disruption, the higher the risk of necrosis.
- Surgical Techniques and Incision Types: The technique used for the breast lift – mastopexy may also impact the likelihood of fat necrosis.
Patient-Related Factors
Patient-specific factors also significantly influence the risk of fat necrosis. These factors include lifestyle choices, underlying medical conditions, and overall health:
- Smoking: Smoking is one of the most well-known risk factors for fat necrosis. Nicotine constricts blood vessels, reducing blood flow and oxygen supply to the tissues. In the context of breast lift – mastopexy surgery, this reduced blood flow can be detrimental, increasing the risk of fat necrosis. Women who smoke are typically advised to quit well in advance of surgery to optimise their blood circulation and healing capacity.
- Underlying Health Conditions: Certain medical conditions, such as diabetes, can affect blood circulation and wound healing, raising the likelihood of complications like fat necrosis. Diabetes, in particular, impairs the body’s ability to heal efficiently and can cause changes in blood vessels that limit adequate blood flow to the tissues involved in the surgery. Other conditions, such as autoimmune disorders or vascular diseases, may also contribute to poor blood supply and increase the risk of necrosis.
- Body Mass Index (BMI): Patients with a higher BMI or those with a significant amount of fatty tissue in the breast may also be at a greater risk. Excess fatty tissue can make it more challenging to maintain adequate blood flow throughout the breast, leading to a higher likelihood of fat necrosis if the circulation is compromised during surgery.
Role of Fat Grafting (if used)
Fat grafting is sometimes combined with breast lift procedures to change breast shape and volume. This technique involves transferring fat from another part of the body (e.g., abdomen or thighs) to the breast. Fat grafting can produce good results, but it also carries a risk of fat necrosis if not done correctly.
- Improper Transfer of Fat Cells: For fat grafting to be successful, the transferred fat cells need to establish a new blood supply in the breast tissue. If these cells do not receive sufficient blood flow, they can die, leading to fat necrosis. This is more likely to happen if the fat is injected in large quantities or in a way that doesn’t allow the cells to adequately integrate with the surrounding tissues.
- Techniques for Reducing Risk: Surgeons skilled in fat grafting use specific techniques, such as injecting small amounts of fat in multiple layers and areas, to ensure the best chance of survival for the fat cells. By carefully distributing the fat and using precise methods, they can help promote blood supply to the grafted cells, minimising the risk of fat necrosis.
Why It’s Important to Seek Medical Attention for Fat Necrosis
Fat necrosis often presents with symptoms such as lumps, skin changes (like dimpling or redness), or even tenderness in the breast. These symptoms can be alarming, as they are similar to those associated with more serious conditions, particularly breast cancer. It is important not to dismiss any breast changes as minor, even if they seem harmless.
The diagnostic process for fat necrosis typically begins with a clinical examination. During this examination, your surgeon will:
- Assess the Lump: Your surgeon will feel the lump or any abnormal area in the breast to determine its size, shape, texture, and mobility.
- Evaluate Other Symptoms: Your surgeon will also check for other signs such as skin dimpling, redness, bruising, nipple discharge, or pain. These symptoms are important to note as they can provide additional clues about the nature of the lump.
The clinical examination is an essential first step in narrowing down the possible causes of the breast changes. However, because fat necrosis can closely resemble other conditions, further diagnostic tests are often required to confirm the diagnosis.
Imaging Tests
If the clinical examination suggests the possibility of fat necrosis, the next step usually involves imaging tests to gain a more detailed view of the breast tissue and the characteristics of the lump. Common imaging techniques include:
- Mammogram: A mammogram is one of the most common imaging tests used to examine breast tissue. It can detect changes in the breast, such as lumps or abnormalities. However, fat necrosis can sometimes appear similar to malignant tumours on a mammogram, making it difficult to differentiate between benign and malignant conditions based solely on this test.
- Ultrasound: An ultrasound uses sound waves to create images of the breast tissue. It is particularly useful in evaluating whether a lump is solid or filled with fluid (as in the case of a cyst). In cases of fat necrosis, an ultrasound may reveal a distinct, well-circumscribed area that is consistent with fatty tissue changes, but this still may not provide enough information to rule out other conditions.
- MRI (Magnetic Resonance Imaging): An MRI provides a highly detailed image of the breast tissue and is often used when the results of a mammogram or ultrasound are inconclusive. An MRI can show the extent of the necrosis and help differentiate it from malignant growths. However, like other imaging methods, an MRI alone cannot definitively diagnose fat necrosis, as its appearance can overlap with that of cancerous tumours.
Imaging tests are valuable tools in the diagnostic process, but they are not always definitive. Fat necrosis and breast cancer can look similar on scans, necessitating further investigation to confirm the diagnosis.
Biopsy
If imaging tests are inconclusive or if there is any suspicion of malignancy, a biopsy is typically recommended as the next step. A biopsy involves taking a small tissue sample from the lump for microscopic examination, and it is considered the most reliable method for diagnosing fat necrosis and ruling out breast cancer.
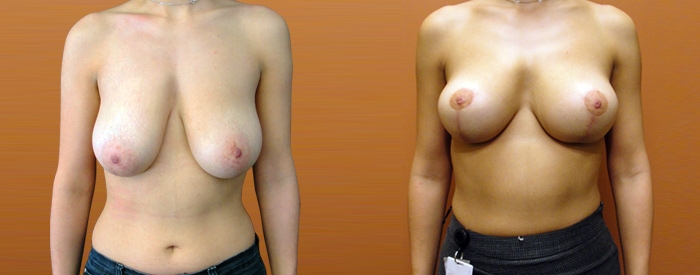
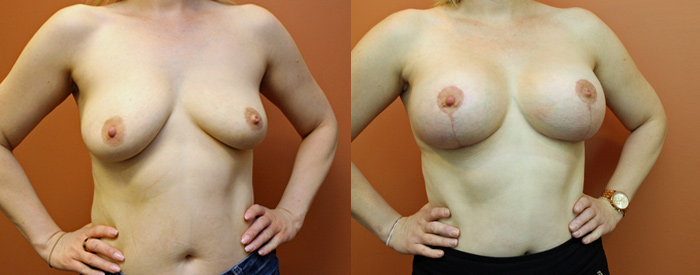
Prevention of Fat Necrosis During and After a Breast Lift
Preventing fat necrosis after a breast lift – mastopexy involves a combination of choosing the right surgeon, taking pre-surgical precautions, employing precise surgical techniques, and following appropriate post-surgical care.
Choosing a Skilled Surgeon
One of the most important steps in preventing fat necrosis is selecting a qualified and experienced surgeon. The expertise and skill of your surgeon directly impact the outcome of the procedure, as well as the likelihood of complications.
Pre-Surgical Considerations
Before having a breast lift, patients can take several proactive steps to reduce their risk of developing fat necrosis. These pre-surgical considerations focus on optimising the patient’s health and preparing the body for surgery:
- Avoid Smoking: Smoking is a significant risk factor for fat necrosis because nicotine constricts blood vessels, reducing blood flow and oxygen delivery to the tissues. Patients are typically advised to quit smoking at least eight weeks before and after surgery to enhance circulation and promote healing. By avoiding smoking, you can reduce the chances of fat necrosis and other complications such as wound healing issues.
- Manage Underlying Health Conditions: Conditions such as diabetes, hypertension, or autoimmune disorders can impair blood flow and healing, increasing the risk of fat necrosis. Proper management of these conditions, including stabilising blood sugar levels and ensuring medications are optimised, can improve surgical outcomes. You should work closely with your primary care physician and your plastic surgeon to ensure that any health conditions are well-controlled before surgery.
- Maintain a Healthy Weight: Patients with a higher body mass index (BMI) or excess fatty tissue in their breasts are at a greater risk of fat necrosis due to potential difficulties in maintaining adequate blood flow. Achieving and maintaining a healthy weight before surgery can minimise this risk and improve recovery. Nutrition, hydration, and physical fitness all play a role in preparing the body for surgery.
Intraoperative Techniques
During surgery, your surgeon’s approach is critical in minimising trauma to the tissues and ensuring sufficient blood flow to the area, both of which are essential in preventing fat necrosis.
- Meticulous Surgical Technique: A skilled surgeon will use precise and meticulous techniques to minimise damage to the tissues and blood vessels. For instance, they may use smaller, strategically placed incisions to reduce the impact on the surrounding tissues and maintain as much blood flow as possible. Gentle handling of tissues is also crucial; by avoiding unnecessary stretching or manipulation, your surgeon can further preserve the integrity of blood vessels supplying the fat.
- Preserving Blood Supply: One of the key objectives during a breast lift – mastopexy is to maintain the blood supply to the breast tissue, especially the fatty areas. This involves carefully planning the incisions and making adjustments during surgery to ensure that the vascular connections remain intact. By optimising the surgical plan to maintain blood flow, your surgeon can significantly reduce the risk of fat necrosis.
Post-Surgical Care
Proper post-surgical care is just as important as the surgical technique itself in preventing fat necrosis. You need to adhere to a comprehensive aftercare plan to ensure optimal healing and minimise complications:
- Wound Care: Following surgery, maintaining proper hygiene and caring for the incision sites is essential to prevent infection and promote healing. You should follow your surgeon’s instructions closely, including cleaning the wound with recommended solutions and keeping it dry. Any signs of infection, such as increased redness, swelling, or discharge, should be promptly reported to your surgeon.
- Monitoring for Complications: Fat necrosis may not appear immediately, so it’s important for patients to monitor their breasts for any changes, such as lumps, skin discoloration, or unusual firmness. Attending follow-up appointments is crucial, as your surgeon will assess the healing progress and check for any signs of fat necrosis or other issues.
- Adherence to Activity Restrictions: Post-surgical activity restrictions are often put in place to avoid putting stress on the healing tissues. Patients are typically advised to avoid heavy lifting, vigorous exercise, and other strenuous activities for several weeks after surgery. Following these guidelines helps prevent trauma to the surgical area and promotes better healing, thereby reducing the risk of fat necrosis.
- Maintaining a Healthy Lifestyle: A nutritious diet and staying hydrated can aid the healing process and enhance tissue recovery. You are encouraged to consume balanced meals rich in vitamins and minerals that support skin and tissue repair, such as vitamin C, zinc, and protein.
Treating Fat Necrosis after Mastopexy
Fortunately, fat necrosis is often a self-limiting condition, meaning it resolves on its own without intervention. However, depending on the size and location of the necrosis, and the severity of your symptoms, various treatment approaches may be considered.
Self-Resolution
In many cases, particularly with minor fat necrosis, the body naturally breaks down and reabsorbs the dead fatty tissue. This process can take several weeks or even months. During this time, you might notice a gradual decrease in the size of the lump and an improvement in any associated symptoms.
While the body works to heal the necrotic tissue, you can take steps to manage any discomfort:
- Over-the-counter pain relievers: These can help reduce pain and inflammation.
- Warm compresses: Applying a warm compress to the affected area can help soothe pain and promote blood flow, potentially aiding in the healing process.
It’s important to note that while these measures can provide temporary relief, they don’t treat the underlying condition. Regular monitoring is still essential.
Medical Procedures
If the fat necrosis doesn’t resolve on its own, causes significant discomfort, or raises concerns about other breast conditions, your surgeon might recommend one of the following procedures:
- Needle Aspiration: This minimally invasive procedure involves inserting a thin needle into the lump to drain any accumulated fluid or oil. It can help reduce the size of the lump and alleviate pressure, but it doesn’t remove the necrotic tissue itself. Sometimes, aspiration needs to be repeated.
- Surgical Excision: In some cases, surgical removal of the necrotic tissue is necessary. This is typically a minor procedure performed under local anaesthesia. Your surgeon makes a small incision and removes the affected tissue. Surgical excision offers a more definitive solution and can provide a tissue sample for biopsy to confirm the diagnosis and rule out other conditions.
FAQs about Breast Lift – Mastopexy and the Risk of Fat Necrosis

How long after a breast lift (mastopexy) can fat necrosis develop?
- Fat necrosis can develop within weeks to months following a breast lift – mastopexy. It’s important for patients to monitor their breasts for any changes, such as lumps or skin irregularities, during the recovery period and beyond. Regular follow-up appointments with your surgeon help detect any complications early.
Is fat necrosis more likely to occur in larger breast lift procedure?
- Yes, patients undergoing larger breast lifts, especially those involving more extensive reshaping and tissue removal, may have a higher risk of fat necrosis due to increased manipulation and disruption of blood supply. Discussing the extent of the surgery and the associated risks with your surgeon can help determine the best approach to minimise complications.
Can wearing the wrong type of bra after surgery contribute to fat necrosis?
- Yes, wearing an ill-fitting or unsupportive bra after a breast lift – mastopexy can potentially impact healing. A proper surgical or supportive bra helps minimise movement and supports blood flow, reducing the risk of complications such as fat necrosis. Dr Lim often recommends specific post-op bras to wear during recovery to promote optimal healing.
Can fat necrosis affect the appearance of the breast lift – mastopexy results?
- Yes, fat necrosis can sometimes cause cosmetic changes, such as indentations, lumps, or asymmetry in the breast, affecting the aesthetic outcome of the procedure. If this occurs, you may need additional treatments or corrective surgery to restore the desired appearance.
Are there lifestyle changes I can make to reduce the risk of fat necrosis before and after my breast lift?
- Maintaining a balanced diet, staying hydrated, avoiding smoking, and managing stress levels can all support better circulation and healing. These lifestyle changes help optimise the body’s ability to recover from surgery and reduce the likelihood of developing complications like fat necrosis.
Further Reading about Breast Lift – Mastopexy with Dr Jake Lim
- Read more about Augmentation Mastopexy – Breast Lift with Implants
- Read more about Breast Lift Techniques – Which One Is Right for You
- Read more about Breast Reduction vs Breast Lift
- Read more about Non-Surgical vs. Surgical Breast Lift (Mastopexy)
- Read more about Breast Lift and Tuberous Breasts